Bipolar: The Descent into Depression
Part 1, Post 2: The Descent into Depression – Understanding the Low Phases
In our previous discussion, we explored how the brain's emotional systems can become overactivated during manic episodes. Now, we turn our attention to the opposite extreme: the depressive phases of bipolar disorder. These periods are not merely episodes of sadness; they represent profound alterations in brain function that can be as debilitating as mania.
The Clinical Landscape of Bipolar Depression
Bipolar depression often presents with persistent low mood, loss of interest in activities, fatigue, feelings of worthlessness, and, in severe cases, suicidal thoughts. Unlike unipolar depression, bipolar depression may also include symptoms such as psychomotor retardation and hypersomnia. These symptoms reflect the complex neurobiological changes occurring during depressive episodes.
Neurobiology of the Depressive Phase
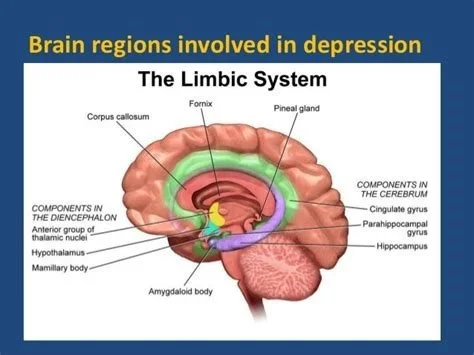
Research indicates that during depressive episodes, there is decreased activity in the prefrontal cortex, a region associated with executive functions and mood regulation. Simultaneously, increased activity in the amygdala, which processes negative emotions, has been observed. Neurotransmitter imbalances, particularly reduced levels of serotonin, norepinephrine, and dopamine, contribute to the symptoms experienced during these low phases.(www.slideshare.net)
The Role of Oxytocin
Oxytocin, a neuropeptide known for its role in social bonding and emotional regulation, has been implicated in mood disorders. Studies have shown that oxytocin levels are elevated during manic episodes and lower during depressive episodes in individuals with bipolar disorder. This fluctuation suggests that oxytocin may play a role in the mood swings characteristic of bipolar disorder. However, the exact mechanisms remain under investigation.
Importance of Early Recognition
Recognizing the early signs of depressive episodes in bipolar disorder is crucial. Each depressive episode can lead to a decline in cognitive and social functioning, some of which may not be fully recovered even during remission. Early intervention can help mitigate these effects and improve long-term outcomes.
Understanding the depressive phases of bipolar disorder is essential for comprehensive management of the condition. In our next post, we will delve into the concept of mixed states, where symptoms of mania and depression coexist, adding another layer of complexity to bipolar disorder.
If you or someone you know is experiencing symptoms of depression or bipolar disorder, it's essential to seek professional help. Early intervention can make a significant difference in outcomes. Call Live Well Psychiatry today to make an appointment.